Lipids are fatty substances found in every cell in our bodies. They make up the membranes that separate the cell from its surroundings and are responsible for regulating the passage of nutrients to and from the cell. One particular family of lipids — sphingolipids — fascinates Prof. Anthony (Tony) Futerman of the Weizmann Institute of Science’s Department of Biological Chemistry. “Sphingolipids were discovered in the 19th century by the German biochemist Johann Thudichum, who named them after the sphinx because they were enigmatic,” says Prof. Futerman.
Although much has been learned about sphingolipids since Thudichum’s time, their role in disease is still being unraveled. Enter Prof. Futerman, who is interested in genetic diseases that cause harmful amounts of sphingolipids to build up in the body’s cells and tissues. People with Gaucher’s (go-SHAYZ) disease, for example, lack an enzyme called glucocerebrosidase. Normally this enzyme breaks down a sphingolipid called glucocerebroside. “But if you’re lacking the enzyme, fatty material accumulates in your body and makes you sick,” says Prof. Futerman, who is one of the world’s foremost Gaucher’sresearchers.

Prof. Anthony Futerman
“At the Weizmann Institute, we’re encouraged to do the kind of science in which we allow our imagination to get the best of us.”
This accumulation of fatty material (glucocerebroside) in tissues can cause enlargement of the liver and spleen, bone disease, anemia, and other serious health problems. Gaucher’s disease is most common in people of Eastern and Central (Ashkenazi) Jewish ancestry.
Currently, many patients with Gaucher’s disease are treated every two weeks with injections of Cerezyme®, a modified form of the glucocerebrosidase enzyme. However, the therapy costs around $200,000 a year for each patient. “There are people who cannot get this therapy because it’s too expensive,” says Prof. Futerman. “We’re attempting to help patients with Gaucher’s by developing effective new — and potentially more affordable — therapies.”
“We’re attempting to help patients with Gaucher’s by developing effective new — and potentially more affordable — therapies.”
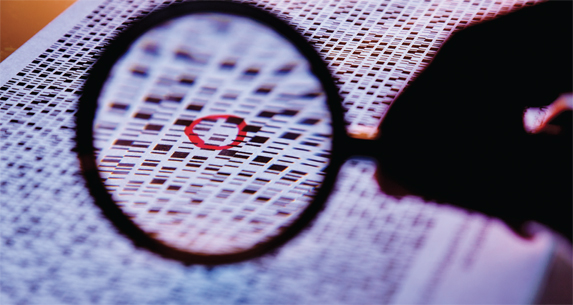
In 2003, he took an important step toward this goal by determining the three-dimensional (3D) structure of glucocerebrosidase. Collaborating with Prof. Joel Sussman of the Department of Structural Biology and Prof. Israel Silman of the Department of Neurobiology, Prof. Futerman and his research team utilized a method called x-ray crystallography to expose crystals of the enzyme to high-intensity x-ray beams. Now that they have detailed information about the structure of glucocerebrosidase, the scientists are focusing on designing a better enzyme. “We’d like to make an enzyme that would last longer, so patients would need far fewer injections,” says Prof. Futerman.
He also wants to find out why some patients with Gaucher’s disease develop neurological problems and others do not. “Little is known about how the accumulation of the sphingolipid leads to neurological defects,” he says. “In our lab, we’re working on understanding the steps in this process using mouse models and cultured cells. Our thinking is: we might be able to come up with a way to intervene in this process, which could lead to the development of a new medication.”
Over the past 20 years, researchers have discovered that sphingolipids are involved in a large number of diseases — such as head and neck cancer and liver cancer — in addition to lipid storage disorders such as Gaucher’s. Prof. Futerman and his colleagues recently began using a mouse model to investigate how the disruption of normal sphingolipid metabolism can lead to liver cancer. “We created a mouse that lacks a particular gene that makes a sphingolipid,” he explains. “As a result, this mouse develops liver cancer.”
Born and raised in London, Prof. Futerman received his PhD from the Weizmann Institute’s Feinberg Graduate School in 1986. After completing postdoctoral work at the Carnegie Institution of Washington (now the Carnegie Institution for Science) in Baltimore, Maryland, he returned to Weizmann in 1990. Today he is the director of the Nella and Leon Benoziyo Center for Neurological Diseases.
Prof. Futerman studies genetic diseases that cause harmful amounts of sphingolipids — named for the sphinx because they are enigmatic — to build up in cells and tissues.
“At the Weizmann Institute, we’re encouraged to do the kind of science in which we allow our imagination to get the best of us,” says Prof. Futerman. External funding agencies, he notes, want to know exactly what a scientist expects to discover when they apply for a research grant. But the Weizmann Institute gives its faculty the freedom to pursue their interests without knowing where their research might lead.
“If, five years from now, we discuss my work, I can’t predict what I’ll be talking about — it will probably have something to do with sphingolipids, but I might have become an expert on cystic fibrosis,” Prof. Futerman says. “Since the Weizmann Institute allows me to do what I want to do, my work will lead me in directions I never would have imagined 10 years ago.
Prof. Anthony Futerman's research is supported by the M.D. Moross Institute for Cancer Research; the Carolito Stiftung; the Adelis Foundation; and the Nella and Leon Benoziyo Center for Neurological Diseases, which he heads. Prof. Futerman is the incumbent of the Joseph Meyerhoff Professorial Chair of Biochemistry.
