Weizmann Institute findings in mice may help explain how viral infection during pregnancy raises the risk of autism and schizophrenia in offspring

REHOVOT, ISRAEL—June 27, 2016—Disrupted fetal immune system development, such as that caused by viral infection in the mother, may be a key factor in the later appearance of certain neurodevelopmental disorders. This finding emerges from a Weizmann Institute study published in Science on June 23.
The study may explain, among other things, how the mother’s infection with the cytomegalovirus (CMV) during pregnancy, which affects her own and her fetus’s immune system, increases the risk that her offspring will develop autism or schizophrenia, sometimes years later. This increased risk of neurodevelopmental diseases was discovered many years ago in epidemiological studies and confirmed in mouse models, and now the Weizmann study – led by Dr. Ido Amit of the Department of Immunology and Prof. Michal Schwartz of the Department of Neurobiology – provides a possible explanation for this increase on the cellular and the mechanistic molecular levels.
“Previous studies had shown that the timing of the disruption in the mother’s immune system during pregnancy affects the type of brain damage her child may develop. For example, a viral infection in early pregnancy raises the risk of autism, whereas an infection later in the pregnancy raises the risk of schizophrenia,” said Dr. Amit. “We’ve set out to examine the mechanisms behind these phenomena, while focusing on the role the immune system plays in brain development.”
Orit Matcovitch-Natan, a graduate student in the laboratories of both Dr. Amit and Prof. Schwartz, and other members of the two teams, studied the sole immune cells present in the brain – the microglia, which contribute to the brain’s development and maintenance. The scientists discovered that the development of these cells in the mouse fetus and in newborn mice proceeds in three distinct stages, parallel to those of the developing brain: early cells that populate the brain of the embryo shortly after its inception, pre-microglia, and adult cells. By screening the genomes of these cells and testing them extensively, the scientists were able to define each stage in terms of its activated genes, their control mechanisms, and the epigenetic features – that is, the activation of proteins that “package” the DNA and affect gene expression in the course of development. The scientists also characterized the functions of some of these genes in the microglia, which contributed to an in-depth understanding of the developmental processes.
The second stage – that of the pre-microglia – proved the most sensitive to disruptions. This stage takes place close to birth and shortly afterwards, just when the developing brain undergoes the vital process of “pruning,” in which inappropriate synapses among neurons are lopped off. The pre-microglia play an important role in pruning, helping remove the superfluous neuronal networks, and shaping and strengthening the connections among the remaining neurons. When the scientists exposed the brains of pregnant mice to synthetic materials that mimic a CMV infection, they found that the development of the pre-microglia was disrupted in their offspring. Genes involved in the maturation of these cells were expressed at the wrong time, and the cells proceeded to an adult stage earlier than usual. The offspring later exhibited abnormal behavior, including disturbances in social interaction and behaviors similar to those of people with schizophrenia.
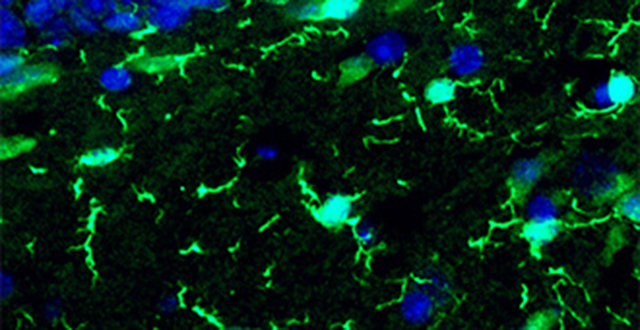
Microglia (bright green) in an adult mouse brain, viewed under a fluorescent microscope
“We’ve discovered that it’s essential for the development of immune cells in the brain to be synchronized with the development of the brain itself,” says Prof. Schwartz. “Premature shift of the microglia in mice to the adult stage leads to brain malfunction later on.” Though these findings have been obtained in mice, the scientists hypothesize that disrupted coordination between the development of the microglia and that of the brain contributes to an increased risk of such neurodevelopmental disorders as autism and schizophrenia in human beings as well. The scientists believe that the heightened immune response to viral infection in the mother’s body may be responsible for disrupting the timing of microglia development.
“Our research has paved the way for studying the effects of other viruses on the mother’s immune system in general, and on her offspring’s brain development. It can also advance the study of neurodevelopmental disorders and their connection to the immune system,” says Orit Matcovitch-Natan.
In yet another series of experiments, the Weizmann scientists established a connection between the development of the microglia in the brains of mice and intestinal microbes – the microbiome. They found that in newborn mice that were free of any microbes, the maturation of the microglia was delayed. This finding suggests that in human babies, factors that shape the microbiome – natural ones such as breastfeeding, or therapeutic ones such as antibiotics – may affect the immune cells in the baby’s brain and consequently the brain’s development. It’s still unknown to what extent this research on mice is relevant to human beings, but the scientists hope that an improved understanding of this process may in the future help prevent certain neurological disorders in babies, caused by disruptions in the mother’s immune system.
Taking part in the study were Dr. Deborah R. Winter, Amir Giladi, Eyal David, and Dr. Hadas Keren-Shaul, as well as Dr. Eran Elinav and Christoph Thaiss of the Department of Immunology, and Hila Ben-Yehuda, Merav Cohen, and Dr. Kuti Baruch of the Department of Neurobiology. Matcovitch-Natan and Amit Spinrad, also a graduate student, belonged to both departments. Study participants also included Prof. Michael H. Sieweke of Centre National de la Recherche Scientifique, France.
Dr. Ido Amit’s research is supported by the Benoziyo Endowment Fund for the Advancement of Science; the David and Fela Shapell Family Foundation INCPM Fund for Preclinical Studies; the Wolfson Family Charitable Trust; the Leona M. and Harry B. Helmsley Charitable Trust; and the Rosenwasser Fund for Biomedical Research. Dr. Amit is the incumbent of the Alan and Laraine Fischer Career Development Chair.
Prof. Michal Schwartz’s research is supported by Sonia T. Marschak, Lincolnwood, IL; Elaine Petchek, Scarsdale, NY; Nathan and Dora Oks, France; and Hilda Namm, Larkspur, CA. Prof. Schwartz is the incumbent of the Maurice and Ilse Katz Professorial Chair of Neuroimmunology.
