REHOVOT, ISRAEL—January 18, 2024—Winning a battle requires precise intelligence and unwavering resolve. But when it comes to the battle against cancer, the immune system’s soldiers – called T cells – quickly become exhausted, and intelligence-providing dendritic cells are scarce. This is one of the reasons why the great promise of immunotherapy – a new generation of treatments that harness the body’s own immune system to fight cancer – has not been fully realized.
However, this could soon change thanks to a new discovery. In a study published today in Cell, Weizmann Institute of Science researchers present a newly developed antibody that connects T cells to dendritic cells, creating a powerful immune response to cancerous growths. The research opens a new avenue in immunotherapy: the development of treatments that link various cells in the immune system to create a powerful team that may be able to defeat cancer and other diseases.
One of the most prominent immunotherapies currently available uses antibodies that block PD-1, a regulatory “checkpoint” receptor found on the surface of T cells. When PD-1 is expressed in T cells, a protein widespread in the tumor environment can attach to it, switching the T cells into a state known as exhaustion. PD-1 antibodies prevent this protein from attaching to T cells and repressing them. Unfortunately, many cancer patients fail to respond to this treatment, or the effectiveness is short-lived.
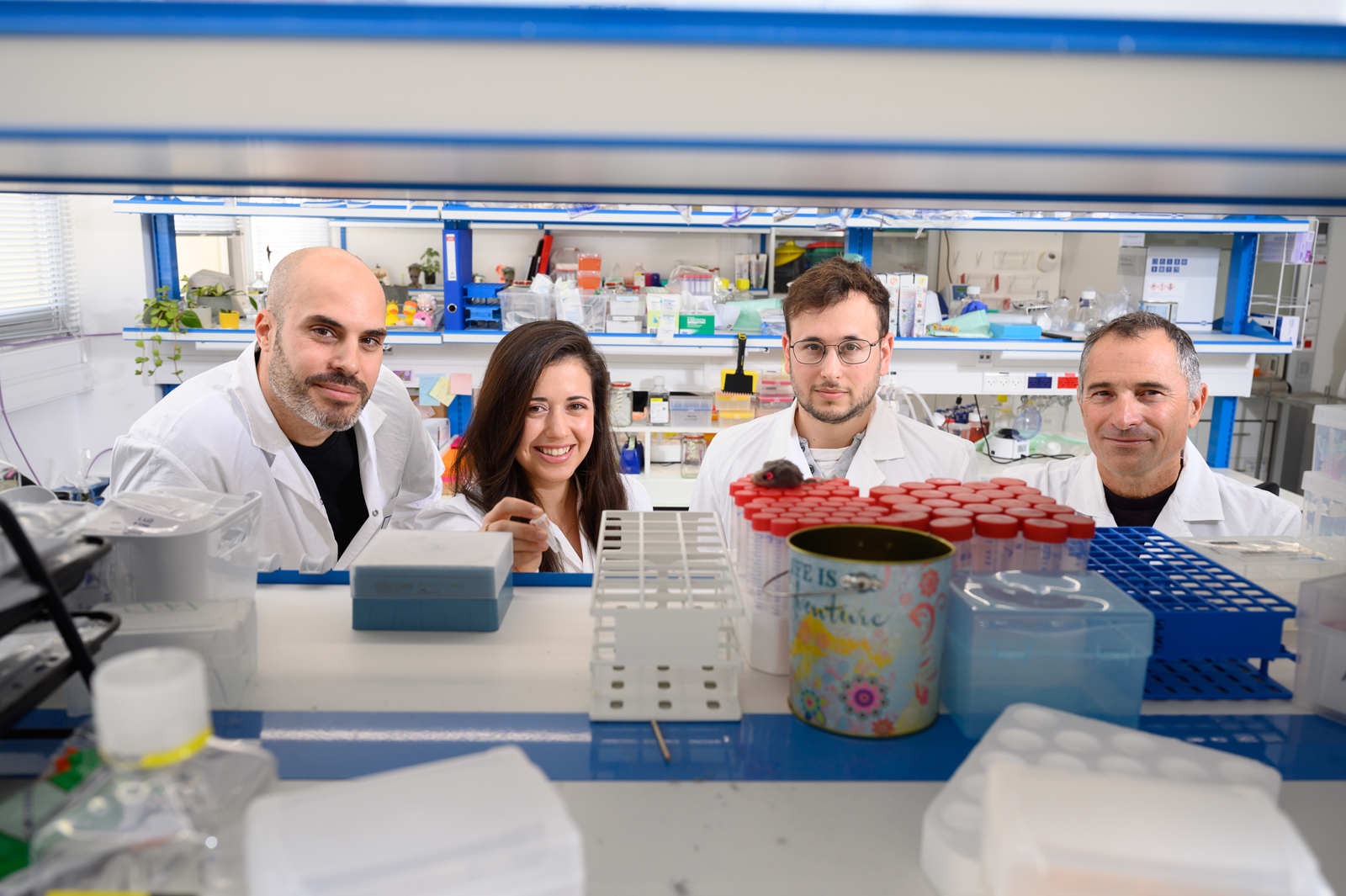
To develop a more effective type of immunotherapy, researchers from the laboratories of Dr. Rony Dahan and Prof. Ido Amit in Weizmann’s Systems Immunology Department set out to learn why existing treatments fall short by sampling T cells from two mouse models of cancer that had undergone PD-1 antibody treatment.
“Using advanced technologies such as single-cell DNA sequencing and big data algorithms, we examined almost 130,000 T cells, some of which responded to the treatment and some of which did not,” Amit explains. “Surprisingly, the group of T cells that did respond to the treatment expressed genes pointing toward an interaction with a rare population of dendritic cells.”
Dendritic cells collect intelligence from across the body by swallowing molecules belonging to malignant cells. They then deliver that information to T cells, warning them about the cancerous growth and prompting them to take action. PD-1 antibodies are supposed to help activate the T cells that fight cancerous growths, but when the researchers examined a cancer model from a mouse lacking dendritic cells, they discovered that the antibody treatment had lost its effectiveness entirely. In other words, dendritic cells are vital to the multiplication and activation of specific T cells in the fight against cancer and are therefore necessary for the treatment as a whole to be successful.
These findings exposed a key weakness in existing treatments: The relevant population of dendritic cells is rarely present in most cancerous growths and in most patients currently being treated with PD-1 antibodies. Under these conditions, interaction between these cells and T cells rarely takes place.
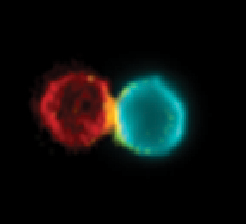
This understanding paved the way for the engineering of a new antibody called BiCE (Bispecific DC-T Cell Engager), which has two arms designed to connect two different types of cells. One arm binds to T cells, inhibiting the PD-1 receptor just as existing treatments do, and the other arm recruits the dendritic cells from the rare population that is vital for activating T cells. The development of the new treatment was led by doctoral research students Yuval Shapir Itai, from Dahan’s laboratory, and Oren Barboy, from Amit’s laboratory.
After creating the antibody, the researchers studied its mechanism of action. When they used fluorescent markers to label the antibody and the immune cells of mice with skin cancer that had been given the new treatment, they were able to observe how the antibody physically connected the T cells to the dendritic cells, increasing the number of such cellular pairs around the cancerous growth and in the adjacent lymph nodes. They also discovered that the cellular pairs created by the antibody were active and that they triggered an immune response against the growth. In the wake of the treatment, the dendritic cells that had been adjacent to the cancerous growth migrated to the lymph nodes and connected to T cells there, sharing intel and activating them.
New hope for untreatable diseases
The effectiveness of this new treatment was tested in several mouse models of cancer, including aggressive breast, lung, and skin cancers. Treatment with the new antibody, as compared to the existing treatment, significantly reduced the growth rate of skin and lung cancers. However, breast tumors that did not respond to the existing treatment also failed to respond to the new antibody. Researchers believe that this is because of the very small number of active dendritic cells around these tumors. To combat this, they tried combining the new antibody with an existing treatment that enhances the activity of dendritic cells around the growth. This combined treatment was more effective than the existing options, proving that even in cancers that had not responded to immunotherapy until now, the synergy between T cells and active dendritic cells creates a powerful immune response against the tumor.
The next stage of the study was to examine whether the new antibody could also prevent the disease from returning. Many cancer patients experience a recurrence even after the primary growth has been removed and metastases have been treated. Often, tiny remnants of the disease escape detection and start developing later, causing the tumor to recur. Unlike existing treatments, BiCE has been found to be effective in thwarting the development of metastases in the lungs after the removal of the primary tumor. This suggests that the antibody creates a systemic immune response against the cancer throughout the entire body and that after treatment, it leaves behind immune cells that remember how to identify the cancer and respond accordingly.
“We are presenting a new approach that puts the emphasis on a system view of immunotherapy. Instead of looking at one avenue, we engineer antibodies that serve as a communication platform between whichever immune cells we choose. This development gives hope not only to cancer patients, who need to have their immune systems activated to fight off the growth, but also to people with other diseases such as autoimmune diseases, in which patients need a suppression of the immune response against their own body." – Dr. Rony Dahan
"There are ways of suppressing the entire immune system, but our new approach should make it possible to suppress or activate a targeted immune response, without the broad and dangerous ramifications of overall suppression and activation of the immune system," Dahan continued.
Yeda Research and Development, which is responsible for commercializing the intellectual property of Weizmann Institute scientists, has filed a patent application and is working to develop an innovative treatment based on the Weizmann antibody.
Also participating in the study were Drs. Ran Salomon, Ken Xie and Eitan Winter of Weizmann’s Systems Immunology Department; Akhiad Bercovich and Prof. Amos Tanay of Weizmann’s Computer Science and Applied Mathematics Department; Tamar Shami and Prof. Neta Erez from Tel Aviv University’s Faculty of Medicine; and Dr. Ziv Porat of Weizmann’s Life Sciences Core Facilities Department.
Prof. Ido Amit holds the Eden and Steven Romick Professorial Chair. His research is supported by the Dwek Institute for Cancer Therapy Research; the Moross Integrated Cancer Center; the EKARD Institute for Cancer Diagnosis Research; the Morris Kahn Institute for Human Immunology; the Swiss Society Institute for Cancer Prevention Research; the Elsie and Marvin Dekelboum Family Foundation; the Lotte and John Hecht Memorial Foundation; and the Schwartz Reisman Collaborative Science Program.
Dr. Rony Dahan holds the Rina Gudinski Career Development Chair. His research is supported by the Moross Integrated Cancer Center.
