REHOVOT, ISRAEL—February 27, 2024—The human brain is a well-guarded control center. Its system of blood vessels is surrounded by a densely packed cellular barrier that prevents most substances from getting in or out. This fortified architecture protects the brain, but it can also stop it from getting help when needed – as in the case of a neurodegenerative disease.
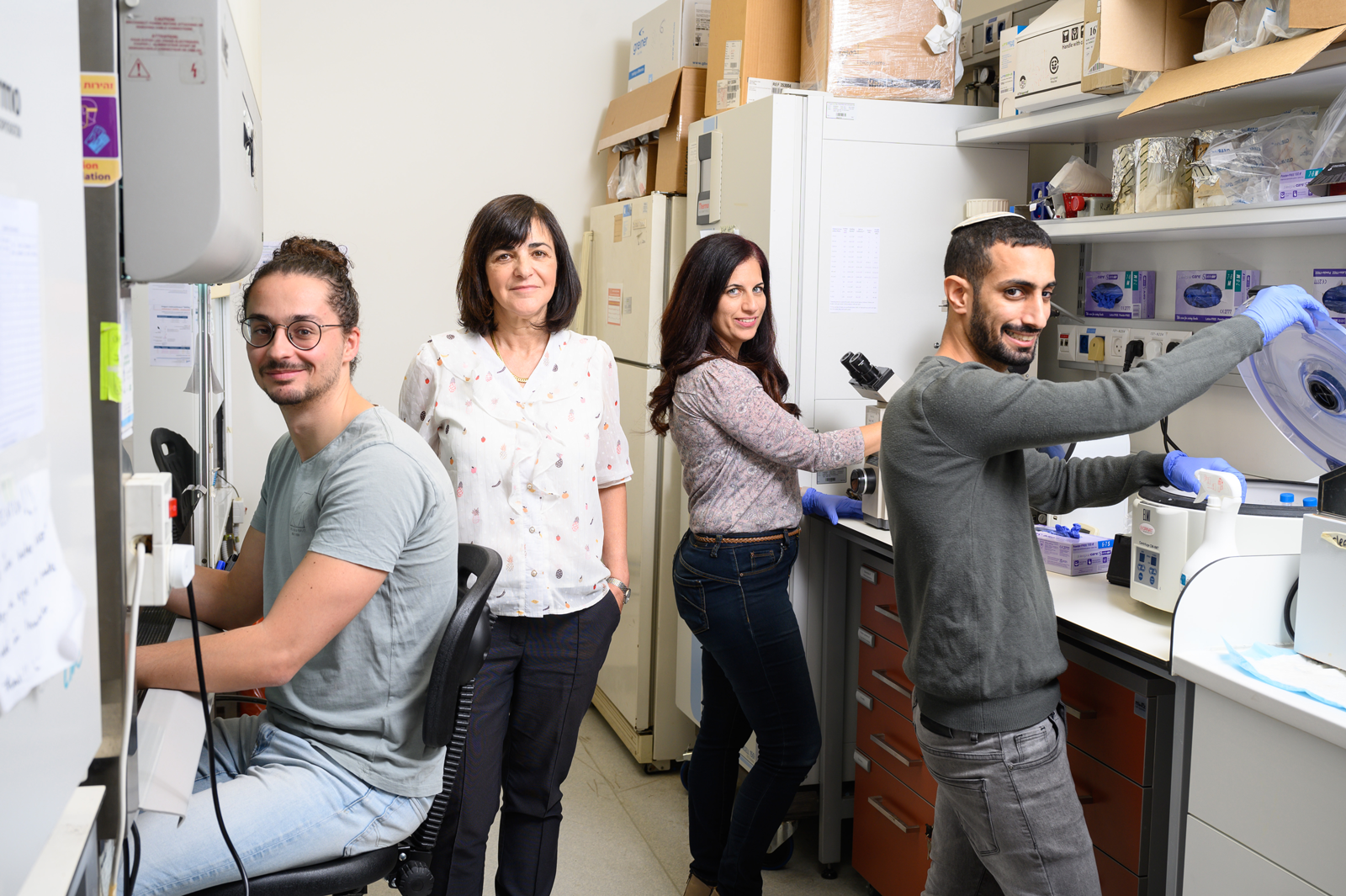
In a new study published in EMBO Molecular Medicine, Prof. Rivka Dikstein of the Weizmann Institute of Science and her team identified two small molecules that manage to penetrate the blood-brain barrier and reduce the levels of a defective protein that causes Huntington’s disease, an incurable neurodegenerative disorder. The new drugs not only slowed the progress of the disease in mouse models but even reversed some of its symptoms.
The signs and symptoms of Huntington’s disease – slight involuntary movements, general clumsiness, and increased anxiety – most commonly emerge around the age of 40. The disease develops over time and inevitably leads to death. It is caused by an excessive repetition, 36 times or more, of a DNA segment in the huntingtin gene. People with Huntington’s usually have one working copy of the huntingtin gene and one defective copy, which leads to the creation of defective proteins that stick together and form a toxic residue in the brain.
This residue accumulates and harms the brain in a number of ways, causing inflammation, thwarting the expression of genes that are vital for the survival of nerve cells, and damaging the cellular power stations called the mitochondria. Previous efforts to treat each mechanism separately were not sufficiently effective, while drugs aimed at tackling the root of the problem – the defective huntingtin protein itself – found it difficult to distinguish the defective protein from the normal one.
A possible ray of hope was discovered in 2019 by Dr. Anat Bahat, a researcher in Dikstein’s lab in Weizmann’s Biomolecular Sciences Department. For years, the lab has been conducting basic research into the Spt5 regulatory protein, a large protein with many functional segments that helps in the production of messenger RNA molecules and is especially important in the production of proteins involved in inflammation.
Bahat and colleagues found that several small molecules can inhibit certain functions of Spt5 without causing significant damage to the protein’s other functions. The researchers then found three small molecules that specifically inhibited the expression of mutant huntingtin without harming the expression of normal huntingtin and other proteins linked to inflammation.
In the new study, Bahat led a team of researchers who examined 17 molecules with chemical structures similar to those found effective in the previous study, in the hope of identifying the most effective inhibitors of mutant huntingtin expression. Using cell cultures from a mouse model of Huntington’s disease, the researchers identified the two most effective molecules. They then tested the new molecules in cell cultures from human patients with varying degrees of genetic defect, and in every case, identified a significant drop in the amount of the mutant protein. At the same time, there was no decrease in the expression of the nonmutant protein – evidence that the new molecules were doing their job with great precision.
The next stage of the study was to test the two selected molecules in genetically modified mice that expressed a fully human version of the mutant huntingtin gene. The mice were treated when they were already exhibiting clear signs of the disease by means of an infusion delivered directly into the damaged part of the brain over the course of four weeks. The treatment reduced the expression of the mutant copy of the gene and increased the proportion of the relevant healthy proteins in the damaged area of the brain.
The treatment also managed to alleviate some of the damage caused by the disease. It increased the expression of two genes that are usually harmed the longer the disease progresses: One is a growth factor essential for nerve cell survival, and the other belongs to the mitochondria. “Even though the aged mouse model simulated the disease at an advanced stage,” Bahat explains, “the treatment succeeded in turning back the hands of time to some extent. In behavior studies, we observed reduced levels of anxiety and improved balance and coordination in the treated mice.”
However, administering an infusion directly into the damaged area of the brain requires a complex surgical procedure that is both risky and painful for patients. The researchers therefore sought to establish whether the drug would be effective if given as a pill or via a subcutaneous injection. They were thrilled to discover that these alternative methods were also successful in reducing the levels of mutant huntingtin in the mice’s brains and that the molecules managed to complete the journey from the mouth or the skin to the brain without undergoing any significant change. Their characteristics allow them to cross the blood-brain barrier and enter the sick area directly once they arrive at their destination.
One of these small molecules demonstrated a healing effect at especially low doses – an important property for a drug designed for human use. The downside, however, was that it had an effect on more than 1,000 other genes. The second molecule required higher doses but proved to be a relatively targeted weapon: It reduced the expression of the mutant gene without causing side effects or any widespread changes to other genes.
In the final part of the study, the researchers examined the effects of the treatment when administered orally over the course of two months at the early stage when the first signs of the disease had only just begun to appear. All of the sick mice exhibited elevated levels of anxiety before the start of the experiment, but for those that received the treatment, anxiety returned to normal levels.
Over time, the loss of balance and the hyperactivity of diseased mice in the control group worsened, while the treated ones had less substantial damage to their balance and did not experience hyperactivity. These findings, coupled with other tests, indicated that the new drugs also delay the disease’s progress when administered at an early stage.
“We were delighted to find that small molecules managed to reach the brain without undergoing changes and without disintegrating along the way,” Dikstein says. “While other experimental treatments require repeated brain or spinal surgery, these molecules, delivered orally or by means of an injection, could pave the way for an effective and safe treatment of Huntington’s disease. In recent years, it’s become clear that a certain function of large regulatory proteins can be precisely targeted using tiny molecules, without harming the overall functioning of these proteins. This understanding could lay the foundations for new treatments for a variety of diseases.”
Also participating in the study were Elad Itzhaki and Dr. Benjamin Weiss of Weizmann’s Biomolecular Sciences Department; Dr. Michael Tolmasov of Bar-Ilan University; Drs. Michael Tsoory and Yael Kuperman of Weizmann’s Veterinary Resources Department; Dr. Alexander Brandis of Weizmann’s Life Sciences Core Facilities Department; and Dr. Khriesto Shurrush of the Medicinal Chemistry Unit in the Nancy and Stephen Grand Israel National Center for Personalized Medicine at the Weizmann Institute.
Prof. Rivka Dikstein holds the Ruth and Leonard Simon Professorial Chair of Cancer Research. She is head of the Y. Leon Benoziyo Institute for Molecular Medicine and of the Dr. Erhard, Emmi and Fred Loewinsohn Center for Pediatric Health. Her research is supported by the Dr. Barry Sherman Institute for Medicinal Chemistry and the Joel and Mady Dukler Fund for Cancer Research.
